Orthognathic Surgery refers to “straightening of the jaw(s) using surgery” [ortho – straight, gnathic – jaw(s)]. Whereas orthodontic treatment corrects the position of the teeth, Orthognathic surgery in Mysore positions the bones of the jaws (maxilla/mandible). One or both jaws may be surgically repositioned during the one operation. This involves making cuts (osteotomies) in the bones and moving the cut segments into their predetermined position under a general anaesthesia. The surgery is normally preceded by a period of orthodontic treatment so that post-operatively both the teeth and the bones will be in their correct position. Finally, a short period of orthodontic treatment is then usually required to complete the alignment of the teeth.
A positive approach is extremely important both before and after jaw correction surgery in Mysuru. Various studies support the fact that positive thinking can assist the body during the process of healing. The support of your family in the days and weeks following your surgery will also aid your recovery.


What is Orthognathic treatment?
An operation is performed by orthognathic surgeon in Mysore to reposition either the upper, lower, or both jaws, in individuals who have a large discrepancy between the size of the jaws in relation to each other, or in whom the jaws are abnormally positioned in relation to the base of skull.
How are people who have these abnormal jaw relationships affected?
Discrepancies between jaw size/position are relatively common and those individuals affected will usually have a malocclusion (poorly aligned teeth and bite) which mostly can be treated using orthodontics (braces) alone. However a small proportion of individuals with severe jaw discrepancies often have significant facial deformity and can be affected in many ways:
- Dental and facial appearance is severely compromised and this leads to high levels of psychological distress, affecting interpersonal relationships and quality of life.
- Jaw function is compromised and this can result in:
- Difficulty eating certain foods in public because it cannot be done in a socially acceptable
- Damage to the gums due to a traumatic bite which may compromise the prognosis of the teeth
- Jaw muscle and jaw joint problems
- Speech difficulties
What causes a jaw discrepancy?
A discrepancy often develops without a specific cause although there may be a family history. Occasionally jaw discrepancies arise as a result of a growth disturbance, for example: following a jaw fracture in childhood or repair of a cleft lip or palate. It can be associated with a syndrome, such as hemifacial microsomia.
A jaw discrepancy may be detected in early childhood but usually becomes more marked during puberty. The unusual jaw growth usually ceases in late adolescence and treatment is directed towards correction of the deformity once growth is complete. Consult jaw correction specialist at orthognathic hospitals in Mysore. A jaw discrepancy may be detected in early childhood but usually becomes more marked during puberty. The unusual jaw growth usually ceases in late adolescence and treatment is directed towards correction of the deformity once growth is complete. Consult jaw correction specialist at orthognathic hospitals in Mysore.
What are the objective, evidence based benefits of the treatment of jaw discrepancies and facial deformity?
- Improvement in oral function (ability to bite and chew)
- Improvement in facial and dental appearance
- Long-term improvement in health-related quality of life, oral health-related quality of life and psychological function
What does the treatment for a jaw discrepancy involve?
Individuals with severe jaw discrepancies usually present to a maxillofacial surgeon or orthodontist following referral by their general dentist in Mysuru. At this stage a diagnosis is made and the patient referred to a multidisciplinary clinic for joint treatment planning with the maxillofacial surgeon and orthodontist at dental hospitals in Mysore.
If, however the patient is still growing they will be reviewed annually until growth is almost complete.
Once facial growth is almost complete (at approximately age 16-18 years) a combined treatment plan will be formulated at a multidisciplinary clinic between the maxillofacial surgeon and orthodontist. Investigations required at this stage will include plain radiographs, plaster models of the teeth, facial and dental photographs. Simulation of the proposed tooth and jaw movements is carried out using cephalometrics (measurement of skull radiographs) in conjunction with treatment planning computer software.
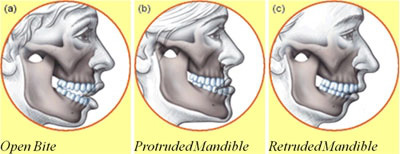
Open Bite
- Speech problems
- Inability to close the mouth naturally
- Long face often
- Often dry red swollen gums
- Chewing problems
- Joint problems
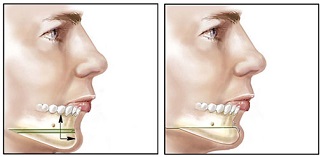
In open bites the upper front teeth are forced outwards-upwards. The front teeth do not touch each other when the mouth is closed. When the bite is closed, only the back teeth meet, while the rest are open. Those people often have a long face, but not always. Open bites often affect speech patterns. There is a difficult lip seal. Furthermore, those people often complain of dry swollen red gums. They sleep with their mouths open (dry mouth and gingivitis). Make an appointment with Dr. Ravi Kumar MP who is the best dental specialist in Mysuru.
Too much teeth showing - Gummy Smile
Synonym: ‘long face’ or ‘vertical maxillary hyperplasia’ (VMH).
Primary cause of a long face is an unfavourable growth pattern (i.e. a developmental growth deformity). Very often, those people have large adenoids. Since their early youth, they had had a clear tendency to sleep with their mouths open and faces in hyper-extension. This caused a stretching vertical outgrow of the face during growth and sleep.
People with long face are the gummy smile, difficulty in closing the lips, and lip strain during mouth closure. The upper jaw has grown vertically too far downwards. When relaxed, the mouth is ‘hanging open’, showing too many teeth. When the patient laughs, there is a disturbing degree of gingival show, resulting in a ‘gummy smile’. In those patients the chin area is often too long and/or the cheek areas are deflated. Here the upper jaw has overgrown vertically in the back area, resulting in an anterior open bite.

In this case Orthognathic surgery in Mysore involves a repositioning of the upper jaw into a higher position in relation to the rest of the face (Le Fort I intrusion osteotomy). Surgical results are often most rewarding. The shape of the face becomes shorter. The restlessness disappears. The smile becomes harmonious. The nose suits the face better. There is a natural closure of upper and lower lips. Sometimes we need to do the surgery on the lower jaw also in order to improve the Facial Aesthetics. Chin surgery is also never far away in the harmonisation of the long face.
Retrognathia Jaw
The word 'retrognathia' is derived from the ancient Greek words retro (backwards) & gnathos (jaw).
Lower jaw too short
Synonym: retrognathia - mandibular retroposition - mandibular retrusion - micrognathism - bird face.
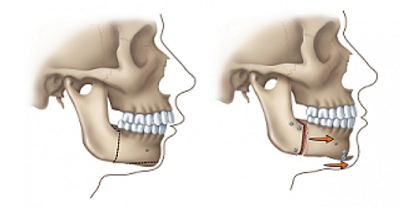
Orthognathic surgery by best orthognathic surgeon in Mysore involves a lower jaw surgery - advancement (BSSO Bilateral sagittal split advancement). A chin advancement procedure is often needed as well.
Upper jaw prognathism
Synonym: Protruding upper jaw.
Upper jaw prognathism is exceptionally rare, yet they are nevertheless split up in two groups.
- Upper jaw prognathism (Maxillary Hyperplasia).
- Alveolar Prognathism (often racial).
Lower jaw too long
Synonym: Lower jaw prognathism, mandibular hyperplasia, protruding lower jaw.

Dental signature for both ‘Protruding lower jaw’ and ‘Receding upper jaw’. The lower teeth are in front of the upper teeth, a condition also called underbite. Both conditions will be discussed under the same heading for reasons that will become clear in further discussion.
Lower jaw prognathism is a genetic-developmental disorder where the lower jaw outgrows the upper jaw, resulting in an extended chin. Mandibular prognathism is a protrusion of the mandible, affecting the lower third of the face. Pure prognathism is corrected by a lower jaw set-back.
Upper jaw too small
Synonym: pseudo-prognathism, maxillary hypoplasia.
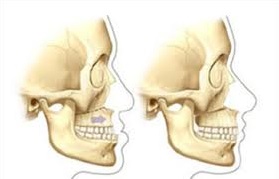
Pseudo-Prognathism or upper jaw hypoplasia is an underdevelopment of the upper jaw and affects the middle third of the face. This condition gives the midface a sunken appearance. It makes the lower jaw stick out, even if it is anatomically normal (= pseudo prognathism - false prognathism).
Maxillary hypoplasia is a developmental growth anomaly, but it may also be the result of poorly planned dental extractions (i.e. iatrogenic) or missing teeth or is a congenital condition as in cleft patients.
Major concern of both conditions are the aesthetics.
Undeniably, both conditions are clinically linked and show more or less the same features. The sunken appearance of the upper jaw or the extended chin of the lower jaw can make a person feel uncomfortable or look sad and depressed, but this may not necessarily be the case.
Corrective surgery is most often carried out on both jaws, not just one jaw. This is merely for aesthetic reasons, but also the consideration of sleep apnea later in life. Jaw corrective Surgery in Mysore aims to reposition the upper jaw and lower jaw is treated with a lower jaw setback and often a genioplasty.
Too less teeth showing
In a short face the upper teeth are hidden behind the upper lip in rest. There are not enough upper teeth on show when the patient laughs or speaks. The upper jaw is vertically deficient and has not developed sufficiently in the vertical dimension.
- Edentulous people also often end up with a short face due to an inappropriate denture.
- Orthognathic surgery is most effective treatment at dental clinics in Mysore in changing the inherent deficient facial proportions.
The Chin
The chin is of vital importance in overall facial aesthetics, as are the cheekbones. The position of the chin influences and directs the whole architecture of the face. Surgery can be done in a single session or as a complement during Orthognathic procedures.

Chin surgery is an essential part of Orthognathic surgery in Mysore, and should be considered in the treatment planning with a yes or a no. If the answer is yes, then the right surgical strategy is the next step. The chin can be made wider or smaller and can be placed forwards or backwards. The chin can be set back, lengthened, or shortened. The chin can be spatially rotated or translated or shaved and remodelled.
Cheek bones
The Zygoma or Cheek bone area is an essential consideration in the overall aesthetic dimension of a face. Unconsciously, we look at the cheekbones in relation to the boundaries of the face. Well defined cheekbones bring out distinction in facial appearance. Prominent malar eminences are a hallmark of beauty in many cultures, and fullness of the malar region conveys a youthful appearance. Flat cheekbones make a person’s face dull and unimpressive, and can even provide a depressive look.
To evaluate the cheekbones more academically, there are several methods published by different authors in the medical literature, some a bit more sophisticated than others.
Cheek bones can be built up permanently using two basic approaches. The two techniques can be combined with no problem.
- Onlay material applied directly to the bone area, this material is intended to become ‘part of the bone’.
- Or tissue filler augmentation (preferably lipofilling) in the cheek’s soft tissues. This fat is intended to become a part of the overlaying tissues. A combination of the two is possible.
Treatment Stages:
Stage 1 Pre-surgical orthodontic treatment:
Orthodontic braces fixed to the teeth are necessary to straighten the teeth in each jaw so that the two jaws can ‘fit’ together properly once the jaw discrepancy has been surgically corrected. This part of the treatment is undertaken by an orthodontist and takes on average about 6 to 12 months depending on the individual case, during which time the patient is seen at regular intervals to adjust the brace.
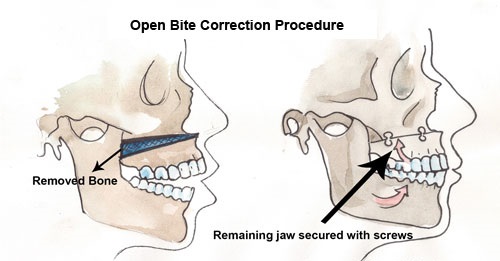
Stage 2 Surgery:
When the orthodontist feels the tooth alignment is satisfactory a final surgical plan will be agreed between the orthodontist and maxillofacial surgeon. Specially trained technicians carry out a simulation of the proposed jaw movements on plaster moulds of the teeth and, if required, construct acrylic splints which the orthognathic surgeon in Mysuru may use at the time of operation to achieve the correct jaw repositioning.
The operation is carried out under general anaesthesia and involves a controlled surgical ‘break’ of either the upper or the lower jaw, or both. The incisions to uncover the bony surfaces of the jaws are normally made inside the mouth thereby avoiding external scars on the face. The mobile jaw fragment/s are then moved into the pre-planned position (using the acrylic splints as a guide), and fixed in the new position using bone plates and/or screws.
The operation at best dental hospitals in Mysore will take between 3-5 hours depending on the complexity of the procedure. Normally patients are cared for as an in-patient but if there are concerns about the airway, some surgeons and anaesthetists care for these patients in a High Dependency Unit (HDU) in the immediate post-operative period. Patients usually stay in hospital between 1 - 3 days post-operatively.
Recovery time is variable but most individuals return to work or study 3 - 4 weeks after the operation.
Stage 3 Post-surgical orthodontic treatment:
Post-surgical orthodontics usually takes about 6 months and is needed to achieve the best possible ‘fit’ of the teeth together. The braces are removed by the orthodontist and the patient is followed up in out-patients for up to 5 years post-operatively.
WHAT ARE THE RISKS OF TREATMENT FOR JAW DISCREPANCIES?
Major problems are rare and Orthognathic treatment in Mysore is a predictable procedure in terms of outcome.
Complications which can occur include:
- Damage to nerves - Following the jaw operation it is common to have transient numbness of the chin, tongue and gums due to ‘bruising’ of nerves in the jaw. In a small number of cases a residual area of numbness remains.
- Damage to the teeth - If teeth are not adequately cleaned, or too many sugary or acidic foods and drinks consumed during orthodontic treatment, the surface of the tooth can be damaged irreversibly.
- Relapse - Although rare, it is possible for the teeth and jaws to relapse (move back towards their original position) to a greater or lesser extent following completion of the treatment. Patients are given retainer braces to minimise this movement of the teeth.
Before Surgery
A pre-anaesthetic consultation and examination, coupled with investigations such as blood tests, may be required before surgery. Your admission to the orthognathic hospital in Mysore is normally on the day of surgery. The necessary anaesthetic and hospital forms need to be completed and returned before this.
If you wish to talk with the anaesthetist before your admission, this can easily be arranged. The anaesthetist may also wish to meet with you beforehand if there are any issues arising from your anaesthetic questionnaire or your pre-operative investigations.
You must not have anything to eat or drink for 6 hours prior to your surgery. If you are a smoker, you are advised to stop two weeks before your operation. On the day of surgery, you should take all your usual medication (unless otherwise instructed) with a small sip of water.
After Surgery
In the vast majority of cases, the jaw bones will be held in their new position by small metal plates and screws. The “hardware” is not normally removed unless it becomes problematic. At the end of the operation, orthodontic elastics may be placed temporarily to guide the jaws together and in doing so, optimise the way that the top and bottom teeth fit together. Rarely, your jaws may need to be wired together.
- Pain - Some pain can be anticipated, but in most cases it is mild to moderate and satisfactorily controlled with analgesic medications. As a comparison, the pain is usually not as bad as that experienced after the removal of wisdom teeth.
- Swelling - Swelling is a normal after-effect of surgery, the degree of which varies between individuals. More swelling usually occurs with lower jaw surgery than with surgery involving the upper jaw, and usually peaks the day after the operation. Your appearance will begin to improve as the swelling resolves. Since almost all the surgery is performed from inside your mouth, your lips will be stretched and slightly abraded, especially at the corners.
- Bleeding - It is common to experience some minor bleeding following surgery, and minor nose bleeds may be expected for a period of one to two weeks following upper jaw surgery. Bleeding into the soft tissues
will produce bruising and this can be quite extensive. In the early stages bruising will be over the jaws but it may spread down the neck and even to the upper chest.
NB: It is unusual for blood loss at the time of surgery to be severe enough to require transfusion, but very occasionally transfusions may be required. Patients may elect to donate some of their own blood beforehand on the off chance that a transfusion is required. Special arrangements must be made several months in advance if this choice is made. - Infection - Infection is possible after any type of surgery. You will be given antibiotics both during, as well as after the operation to help prevent this. If an infection should develop it is usually very easily treated.
- Tingling/Numbness - You will experience altered sensation or numbness, particularly in the lower lip/chin in association with lower jaw surgery; and in the upper teeth following an upper jaw procedure. While the nerve fibres are healing, you may encounter strange sensations or tingling. Normal sensation usually returns in six months or less.
- Mobilising & Breathing Exercises - You will be encouraged to get out of bed, sit up and walk around as soon as possible following the surgery. You will also be asked to take frequent deep breaths to help your lungs recover from the anaesthetic. The earlier you are up and about, the more normal you will feel.
- Clear Fluids - As soon as possible after surgery, you will be encouraged to drink clear fluids. You will usually be able to drink directly from cup or glass and the use of a straw is rarely necessary. Sometimes the use of a special “feeding cup” may be recommended by best dentist in Mysuru. It is important that you drink adequately so the intravenous fluids may be discontinued.
- Tooth Cleaning - You will be encouraged to brush your teeth four to six times per day, especially after eating, paying particular attention to keeping the brush in direct contact with the teeth. Usually a small (children’s size) soft toothbrush is sufficient. In addition to brushing, a mouth rinse should be used. A Chlorhexidine mouthwash is the most effective antibacterial mouthwash and should be brushed onto the teeth and orthodontic appliances.
- Speech - The ease with which you can communicate and be understood is variable; however your speech will improve with practice. It is important that you try to speak more slowly, concentrate on each word and be willing to persevere.
- Nasal Congestion - Nasal congestion may occur both from the tube(s) placed in the nostrils during surgery and also from surgical procedures involving the upper jaw. When this occurs, the congestion can be managed by using nasal sprays and cleansing the nostrils. Cotton buds soaked in warm water may be used to remove nasal secretions. If a nasal spray is required, it should be sprayed with sufficient force for you to taste the medication. Relief should occur in 3-5 minutes. The nasal congestion will usually resolve 1 to 2 weeks after surgery at dental hospitals in Mysuru.
- Jaw Stiffness & Jaw Joint Noises - After Orthognathic surgery in Mysore, the jaw joint will be stiff for several months. The best exercise to overcome the stiffness is normal jaw activity such as chewing. Sometimes clicking or grating noises in the jaw joint may occur as the jaw begins to function. These noises may be permanent but do not usually affect jaw function.
- Post-Surgical Movement (Relapse) - When teeth and jaws are moved by orthodontics and surgery, the goal is to place them in a more favourable position. Many forces have been responsible for the growth and consequent positioning of the jaws and teeth. The muscular forces that caused the original growth problem and the jaw relationship are still present. As a result, there is a small chance that the jaw(s) and teeth will move back towards their original position. This is termed relapse. Many things are done throughout treatment to counteract relapse, but some degree of relapse almost always occurs.
Discharge Home
Most patients are ready for discharge from hospital 2-3 days after their surgery. For the first few days after arriving home, it is essential you have somebody with you to help you with your diet and your general needs.
Medication
Analgesics (pain relief medication), an antibiotic, and a mouthwash will usually be prescribed. Some patients will also be prescribed a nasal spray as discussed.
Diet
You will be provided with detailed dietary information, but feel free to improvise as much as you like. As your food will initially be in liquid form, there is a reduced amount of fibre. This may result in several days of constipation following the surgery. Fruit juices (especially, prune juice) are effective laxatives. Should these measures fail, mild liquid laxatives are available at pharmacies without prescription.
Follow-Up Appointments
A review appointment will be made, usually 1 week after the surgery by best orthognathic surgeon in Mysuru. This is normally followed by appointments at approximately 1 month, 3 months and 1 year post-operatively, at which time further facial x-rays are taken. You will also continue to see your orthodontist afterwards and they will usually take more study models and photographs after 3 months.
FAQ's – ORTHOGNATHIC SURGERY (CORRECTIVE JAW SURGERY)
Are you doing research about jaw surgery? Many of our patients ask similar questions, so we have put together an FAQ to help you as you set out to learn what you need to know about this type of oral procedure. If doubts remain, please do not hesitate to get in touch with our centre to learn more.
Why May I Need Jaw Surgery?

Corrective jaw surgery, also known as Orthognathic surgery, may be required to correct issues in the jaw resulting from its structure, TMJ, issues caused at birth, teeth grinding and clenching (bruxism), sleep apnea, cleft palate, growth deformities, and others.
Who Performs Jaw Surgery?
Corrective jaw surgery is a special type of procedure performed specifically by an oral and maxillofacial surgeon (OMS) or orthognathic specialist in Mysore. You may receive a referral from your general dentist or doctor or find an OMS on your own. Dr. Ravi Kumar is a specialist with 10 years of experience in Orthognathic surgery.
What Are the Symptoms of Someone Who Needs Jaw Surgery?
Jaw surgery can have a dramatic impact on your life, but some patients may not realize they could benefit from it. Some of the signs that you have a condition requiring jaw surgery could include the following:
- Pain in the jaw when eating, speaking, or opening the mouth wide
- Wear and tear of the teeth
- Imbalanced bite
- Mouth breathing
- Sleep apnea
- Protruding chin
- Open bite (when the upper and lower jaw do not fully meet)
- Difficulty breathing
- Birth defects
- Facial trauma
What Can I Expect From Jaw Surgery?
This is surgery that is performed in a hospital. It will usually require you to be put to sleep. The exact treatment plan will depend on your specific needs, but in all cases an incision is made in the inside of the mouth.
What Is Recovery Like after Jaw Surgery?
We will give you precise instructions for recovery before the procedure and once again after. You should maintain a soft foods diet if instructed to do so, take all pain medication as instructed, and get plenty of rest and relaxation. Keeping your head elevated in the hours following the procedure will reduce swelling. Do not hesitate to get in touch with our centre if symptoms persist or do not improve after several days.
Where Can I Learn More about Jaw Surgery?
If you have been told you need to have jaw surgery and are interested in learning more from true experts in oral and maxillofacial surgery, you are invited to contact Dr Ravi Kumar in Precision Centre and request an appointment today.

